Previous Speakers

Mouhanad Hammami
Chief Wayne County Health , Michigan USA

Nikolaos Zacharias
University of Texas Health Science Center USA

Michael Kamrava
Harvard Medical School USA

Dan C. Martin
University of Tennessee Health Science Center USA
Rajeshwar Rao Tekmal
Director, Division of Reproductive Research University of Texas Health care, USA University of Texas Health care, USA

George Peery
Dean University of Texas USA

Ali Ahmad
Consultant NHS UK

Michael Kleerekoper
Professor of Medicine University of Toledo USA
Recommended Global Surgery Webinars & Conferences
Europe & UK
Asia Pacific & Middle East
Canada
Gynecologicalsurgery-2018
About Conference
We are honoured to personally welcome everyone who is related to the 6th American Gynecological Surgery Conference on September 28-29, 2017 at San Antonio, USA. It’s an exciting time for ConferenceSeries Ltd as we continue to grow and adapt, remaining always adaptable, motivated and responsive. The Journey of Global events is an exciting one in which to work, socialize and we’ll continue to meet and bring inspired people together in forums like this, to ensure ConferenceSeries Ltd remains at the cutting edge.
To give you a brief update on where we are today. Conference Series is an open resource platform that conducts 3000+ global events including International Conferences, Workshops, Symposia, Trade Shows, Exhibitions and Science Congresses in all the major scientific disciplines, including Clinical, Medical, pharmaceutical, Engineering, Technology, Business Management and Life Sciences across America, Europe, The Middle East, and Asia Pacific. It is reaching over 25 million researchers, scholars, students, professionals and corporate entities all over the globe
Gynecological Sugery-2018 includes prompt keynote presentations, Oral talks, Poster presentations and Exhibitions. Gynecological Surgery-2018 is designed in interdisciplinary manner with a multitude of tracks to choose from every segment and provides you with a unique opportunity to meet up with peers from both academia and industry, to establish a scientific network between them
A comprehensive range of topics will be discussed in the event including Robotic and Laparoscopic surgery, Puberty, Adolescent and Pediatric Gynecology, Cancer in Gynecology/ Gynaecologic Oncology, Operative Gynecology, Menopause, Maternal/Fetal medicine, Reproductive endocrinology and infertility, Urogynecology/reconstructive pelvic surgery, Sexual Medicine and Infectious Diseases in Gynecology (Acute and chronic), Therapies in Gynecology, Contraception and Family Planning, Midwifery. At Conference Series, It is our ideology to bring maximum exposure to our attendees, so we make sure the event is a blend which covers professionals such as gynecologists, obstetricians, veteran researchers, women healthcare professionals from academia &industry making the conference a perfect platform.
We thank everyone for attending our conference and bringing your expertise to our gathering. You, as organization leaders, have the vision, the knowledge, the wherewithal and the experience to help us pave our way into the future. You are truly our greatest asset today and tomorrow, with your leadership and support we hope to reach further heights and to accomplish more. I ask you to stay engaged and connect with us; help us shape the future of Conference Series Ltd. Our personal thanks and respect goes out to all of you.
Why to attend???
With members from around the world focused on learning about Gynecological Surgery and its advances; this is your best opportunity to reach the largest assemblage of participants from the Gynaecologic community. We conduct presentations, distribute information, meet with current and potential scientists, make a splash with new discoveries in the breast cancer treatment and diagnosis, and receive name recognition at this 3-day event. World-renowned speakers, the most recent techniques, developments, and the newest updates in women’s health, breast cancer, gynaecological issues, pregnancy, Woman Psychology, women disorders are hallmarks of this conference.
Target Audience:
Gynecologists
Nurses
Midwives
Women’s Healthcare Students, Scientists and professors
Breast Cancer surgeons, pathologists
Women’s health Care Researchers
Healthcare Faculty
Medical Colleges
Healthcare Associations and Societies
Business Entrepreneurs
Training Institutes
Software developing companies
Manufacturing Medical Devices Companies
Data Management Companies
Session Tracks
Track 1: Breast cancer and surgery
Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, fluid coming from the nipple, or a red scaly patch of skin. In those with distant spread of the disease, there may be bone pain, swollen lymph nodes, shortness of breath, or yellow skin.
Surgery involves the physical removal of the tumor, typically along with some of the surrounding tissue. One or more lymph nodes may be biopsied during the surgery; increasingly the lymph node sampling is performed by a sentinel lymph node biopsy.
Standard surgeries include:
Mastectomy: Removal of the whole breast.
Quadrantectomy: Removal of one-quarter of the breast.
Lumpectomy: Removal of a small part of the breast.
Once the tumor has been removed, if the patient desires, breast reconstruction surgery, a type of plastic surgery, may then be performed to improve the aesthetic appearance of the treated site. Alternatively, women use breast prostheses to simulate a breast under clothing, or choose a flat chest. Nipple prosthesis can be used at any time following the mastectomy.
Related conference:
Breast Pathology 2018, Conference on July 25-26, 2018 Vancouver, Canada
Breast Cancer 2018, Congress on May 10-11, 2018 Frankfurt, Germany
Breast Cancer Congress 2018, on May 25-26, 2018, New York, USA
Breast Cancer Summit 2018, on July 16-17, 2018 Melbourne, Australia
Womens Health 2018, Conference on August 09-10, 2018 Abudhabi
Breast Cancer Summit 2018, on July 16-17, 2018 Melbourne, Australia
Trauma 2018, Congress on February 22-23, 2018 Paris, France
Healthcare Asia Pacific 2018, Meeting on March 12-14, 2018 Singapore
Nursing Global 2018, Symposium on March 01-03, 2018 London, UK
Track 2: Gynecologic Cancer Surgeries
It is estimated that in America every six minutes a women is diagnosed with cancer and there will be 91730 new cases diagnosed this year alone. Women are often unaware of the signs and symptoms of these cancers and because of this these cancers are called silent killers. Sadly out of the 91730 new cases diagnosed this year, 28080 deaths are predicted.
The uncontrolled growth and spread of abnormal cells are originated from the reproductive organs are called gynecological cancers. Several gynecological cancers include cervical cancer, ovarian cancer, uterine/endometrial cancer, vaginal cancer, vulvar cancer. Surgeries of reproductive cancer include-ovarian cancer surgery, -vaginal surgery, -cervical cancer surgery, Uterine cancer surgery
Related Conferences:
Oncology Research 2018, Meeting on May 10-12, 2018 Frankfurt, Germany
Oncologists 2018, Conference on May 24-25, 2018 Osaka, Japan
Breast Cancer Summit 2018, on July 16-17, 2018 Melbourne, Australia
Gynecologic Oncology 2018, Congress on July 18-19, 2018 Atlanta, Georgia, USA
Euro Cancer 2018, Summit on July 23-25, 2018 Rome, Italy
Cancer Science 2018, Meeting on August 09-10, 2018 Madrid, Spain
Radiology 2018, Conference on Aug 27-28, 2018 Toronto, Canada
Cancer Congress 2018, on September 17-18, 2018 San Diego, California, USA
World Cancer 2018, Symposium on October 11-13, 2018 Zurich, Switzerland
Robotic Oncology 2018, Conference on October 26-27, 2018 Osaka, Japan
Track 3: Minimal invasive surgeries
These surgeries have been enabled by the advance of various medical technologies. Minimal invasive surgical techniques that limit the size of incision needed and reduce the wound healing time associated with pain and risk of infection. Compared to normal open surgeries these minimally invasive surgeries are done in benefit the patient and reduce the cost of surgeries.
Types of surgical procedure are
Myomectomy
Hysterectomy
Other Surgical Procedures:
Diagnostic laparoscopy
Microlaparoscopic pain mapping
Laparoscopic removal of endometriosis
Laparoscopic removal of ovarian cysts
Laparoscopic removal of adhesions (scar tissue)
Laparoscopic removal of a tube and ovary
Laparoscopic uterine suspension
Hysteroscopic surgery (removal of polyps or fibroids from the inside of the uterus)
Laparoscopic bladder support surgery
Endometrial ablation (for heavy periods)
Robotic Assisted Laparoscopic Removal of Fibroids
Related Conferences:
Pediatric Surgeons 2018, Congress on August 13-14, 2018 Osaka, Japan
Orthopedics-2018, Symposium on August 31st - September 1st, 2018, Toronto, Ontario, Canada
Surgery Asia Pacific 2018, Conference on November 27-28, 2018 Singapore
Neurologists 2018, Meeting on November 01-03, 2018 Brussels, Belgium
Automation And Robotics 2018, Symposium on April 16-17, 2018 Las Vegas, USA
Neurosurgery 2018, Congress on April 23-24, 2018 Rome, Italy
Cardio-Thoracic Surgery 2018, Conference on June 06-07, 2018 Osaka, Japan
Surgery Congress-2018, on August 27-28, 2018 Tokyo, Japan
Robotic Oncology 2018, Conference on October 26-27, 2018 Osaka, Japan
Robotic Surgery 2018, Meeting on May 21-22, 2018 Tokyo, Japan
Track 4: Benign tumors in gynecology
These tumors lack the ability of invade neighbouring tissue or metastasize. These are sometimes very larger in size and they don’t grow back when they are removed. Benign tumors generally have slow growth rate than malignant tumors.
Key concepts:
Benign Ovarian Mass
Uterine Mass
Inflammatory Masses
Pregnancy
Benign Tumors vs Malignant Tumors
Related Conferences:
Breast Pathology 2018, Congress on June 25-26,2018 Vancouver, Canada
Gynecology and Obstetrics Pathology 2018, Meeting on March 30-31, 2018 Orlando, USA
Midwifery 2018, Conference on September 26-27, 2018 Chicago, USA
Endocrinology 2018, Summit on October 17-18, 2018 Las Vegas, USA
Nursing & Healthcare Congress 2018, on April 23-25, 2018 Dubai, UAE
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Cancer Science 2018, Meeting on August 09-10, 2018 Madrid, Spain
Cancer Congress 2018, on September 17-18, 2018 San Diego, USA
Cancer 2018, Symposium on October 03-04, 2018 Los Angeles, California, USA
World Cancer 2018, Conference on October 11-13, 2018 Zurich, Switzerland
Track 5: Surgical treatments for female infertility
The female factors of infertility can best be discussed as they affect these various stages.
PHYSIOLOGICAL FACTORS ININFERTILITY:
(1) Reproductive power. Apparently healthy individuals differ widely in reproductive power.
(2) Age. Duncan in 1884 showed that the maximum fertility was between the ages of 20 and 24 years and that after 39 years fertility declined very rapidly.
(3) Stage of menstrual cycle-Fertility varies greatly according to the stage of the menstrual cycle, and there is evidence that the ovum after ovulation remains capable of fertilisation for a few hours only.
INTERFERENCE WITH UNION OF OVUM & SPERM.
(A) Vulva & Vagina.
(1) Thickened hymen.
(2) Congenitally small vaginal introit us and vaginal strictures.
(3) Other causes of Dyspareunia Vulvitis, vaginitis, veganism’s inflammation of Bartholin's glands. Urethral caruncle.
(B) Cervical barriers:-these are primarily Physiological.
(1) Abnormal cervical mucus. The character of the cervical mucus may be altered by an unhealthy
Cervix as evidenced by endocervicitis, erosion or polypi. The mucus becomes purulent and is inimical to the spermatozoa.
(C) Uterine conditions.
(1) Displacement-Mobile retroverted uteri are not a significa11t cause Of sterility. Fixed retroversions, however, which are associated with chronic salpingitis, pelvic peritonitis, or endometriosis, are a common cause of sterility.
(2) Uterine Fibromyomata are found in 3 to 50, 1" of women complaining of infertility.' According to Read, cornual or submucous tumours may cause infertility by occlusion of the tubes, distortion and enlargement of the uterine cavity and their association with chronic endometrial hyperplasia.
(3) Hypoplasia of the uterus associated with hypoplasia of the vagina, cervix and ovaries is an important cause of sterility, all the more so, because in some cases it may be prevented. The cause may be anything that retards the growth of the endocrine glands during embryonic life, infancy, childhood or puberty.
(4) Disordered uterine action. Attention was first drawn to the relation of this functional disturbance
To infertility by Stall worthy, who described the female genital tract as the most hysterical portion of a woman's anatomy. This is manifested in undue uterine and tubal irritability, as can be emonstrated by tubal insufflation of hysterosalpingography,
Related Conferences:
Thyroid 2018, Conference on September 03-04, 2018 Auckland, New Zealand
Diabetes 2018, Conference on September 28-29, 2018 Montreal, Canada
Endocrinology Summit 2018, on October 01-02, 2018 Osaka, Japan
Euro Endocrinology 2018, Meeting on November 26-27, 2018 Dublin, Ireland
Anesthesiology-2018, Symposium on November 15-16, 2018 Dubai, UAE
Surgery Asia Pacific 2018, Conference on November 27-28, 2018 Singapore
Gynecology and Obstetrics Pathology 2018, Symposium on March 30-31, 2018 Orlando, USA
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Anesthesiology-2018, Conference on November 15-16, 2018 Dubai, UAE
Surgery Asia Pacific 2018, Conference on November 27-28, 2018 Singapore
Gynecology and Obstetrics Pathology 2018, Symposium on March 30-31, 2018 Orlando, USA
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Track 6: Robotic and Laparoscopic surgery:
Laparoscopic surgery is subject to certain limitations that can be a problem when performing complex minimally invasive operations. Robotic surgery was developed precisely to overcome such technical limitations. The question therefore arises whether robotic surgery leads to significantly better results compared with standard laparoscopic surgery.
Laparoscopic surgery has certain limitations. Like two-dimensional imaging, restricted range of motion of instruments, and poor ergonomic positioning of the surgeon. To solve these problems robotic system was introduced and to minimize the shortcomings of laparoscopy. The two major features of robotic-assisted laparoscopic surgery are improved visualization and greater dexterity.
United States cleared the intuitive Surgical’s da Vinci system, which was discussed in 4000 peer-viewed publications. Medical robotics is causing a paradigm shift in therapy. Food and Drug Administration (FDA) for multiple categories of operations, and was used in 80% of radical prostatectomies performed in the USA in 2008; just 9 years after the system went on the market. Robotic prostatectomy is now the standard of care.
Based on the nationwide inpatients sample Data project per 10,000, robotic surgery had lower mortality rate than non-robotic surgical procedures. Robotic surgery also had short hospital stay than open surgery in all sub-groups. Robotic surgeries reduce the charges Median ($ 30,540) than laparoscopic ($ 34,537) and open surgery ($46,704).
Related conferences:
Surgery Asia Pacific 2018, Conference on November 27-28, 2018 Singapore
Neurologists 2018, Conference on November 01-03, 2018 Brussels, Belgium
Automation And Robotics 2018, Meeting on April 16-17, 2018 Las Vegas, USA
Neurosurgery 2018, Symposium on April 23-24, 2018 Rome, Italy
Cardio-Thoracic Surgery 2018, Conference on June 06-07, 2018 Osaka, Japan
Surgery Congress-2018, on August 27-28, 2018 Tokyo, Japan
Robotic Oncology 2018, Summit on October 26-27, 2018 Osaka, Japan
Robotic Surgery 2018, Conference on May 21-22, 2018 Tokyo, Japan
Breast Pathology 2018, Summit on June 25-26,2018 Vancouver, Canada
Gynecology and Obstetrics Pathology 2018, Conference on March 30-31, 2018 Orlando, USA.
Track 7: Puberty, Adolescent and Pediatric Gynecology
It is being increasingly recognized as a fact that gynaecologic disorders can have their origin in childhood disorders such as congenital defects, neglected infections acquired in childhood, failure to diagnose and treat endocrinopathies in childhood, tumours overlooked and a general tendency to belittle physical and psychological trauma of sexual abuse. All these can cast their shadow on future reproductive health of the individual during adult life. The understanding of the role of the gynaecologist in the timely detection of these problems, instituting preventive and timely therapeutic interventions to correct the same if possible and counselling the parents about the likely squeal as well as measures to mitigate their consequential ill-effects can all contribute towards improving the future quality of life. These should be the goals of the clinician practicing this subspecialty.
Common Paediatric Gynaecologic Problems
The prepubertal girl child: The common problems for which medical opinion is sought include broadly:
Vulvovaginal infections and leucorrhoea
Vaginal bleeding
Ambiguous genitalia
Abdominal neoplasms
Sexual abuse
Sex education—sexuality
Related conferences:
Breast Pathology 2018, Meeting on June 25-26,2018 Vancouver, Canada
Gynecology and Obstetrics Pathology 2018, Conference on March 30-31, 2018 Orlando, USA
Midwifery 2018, Summit on September 26-27, 2018 Chicago, USA
Neonatal Nursing Congress 2018, on May 14-15, 2018 Singapore
Midwifery Congress 2018, on May 11-12, 2018 Osaka, Japan
Breast Cancer 2018, Conference on May 10-11, 2018 Frankfurt, Germany
Nursing Global 2018, Symposium on March 01-03, 2018 London, UK
Hormone 2018, Conference on December 13-14, 2018 Dubai, UAE
Endocrinology 2018, Meeting on October 17-18, 2018 Las Vegas, USA
Nursing & Healthcare Congress 2018, on April 23-25, 2018 Dubai, UAE
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Track 8: Cancer in Gynecology/ Gynaecologic Oncology
Women are at risk of gynecologic cancers and risk increases with age. Risk can be lowered if they are found early and treated. The five main cancers affect women’s reproductive organs are cervical, ovarian, utrerine, vaginal and vulvar. All these cancers referred as gynaecologic cancers as a group. Each cancer is unique with different symptoms and risk factors. There are many other tumours such as Benign Tumours of the Genital tract, Benign Tumours of the Cervix, Benign Tumours of Uterus
Benign Tumours of the Genital Tract: recognises and evaluates tumours of the genital tract so that appropriate management can be instituted.
Demonstrates knowledge of the common infective and benign tumours which may be found in the genital tract.
Differentiates between common infective and non-infective tumours of the genital tract.
Discusses the clinical features of benign tumours of the genital tract.
Makes and discusses a provisional diagnosis of a benign tumour of the genital tract.
Indicates the management of choice of benign tumours of the genital tract.
Cancers of Endometrium, Uterus and Fallopian Tube
Endometrial Cancer
Risk Factors for Endometrial Cancer
Endogenous oestrogen dependent
Nulliparity, low parity
Polycystic ovary syndrome (PCOS)
Early menarche, late menopause
Functioning ovarian tumours
Obesity, hypertension, diabetes, hyperlipidaemia
Exogenous oestrogen
Unopposed oestrogen therapy
Tamoxifen
Other risk factors
Hereditary
Sarcoma of the Uterus
Choriocarcinoma
Fallopian Tube Cancer
Related conferences:
Cancer Science 2018, Conference on August 09-10, 2018 Madrid, Spain
Cancer Congress 2018, on September 17-18, 2018 San Diego, USA
Cancer 2018, Conference on October 03-04, 2018 Los Angeles, California, USA
World Cancer 2018, Summit on October 11-13, 2018 Zurich, Switzerland
Cancer Therapy-2018, Symposium on October 29-30, 2018 San Francisco, California, USA
World Cancer 2018, Summit on July 02-03, 2018 Thailand, Bangkok
Medical Oncology-2018, Meeting on May 28-30, 2018 Osaka, Japan
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Advanced Nursing Science 2018, Conference on April 20-21, 2018 Las Vegas, USA
Track 9: Operative Gynecology
Surgical procedures have become very safe today, because of improved anaesthesia, availability of blood transfusion, antibiotics as well as good preoperative and postoperative care of the woman. Advanced surgical technologies have also contributed to reduced surgical morbidities and operation-related complications.
It is therefore important to pay due attention to pre-operative and postoperative management of a woman undergoing surgery.
Preoperative Investigations: Prior to the submission of the patient to any major gynaecological surgery, it is necessary to evaluate her fitness for it. The preoperative investigations include the following:
Complete blood count. This includes haemoglobin assessment and total and differential leucocyte count.
Urinalysis. This includes routine and microscopy urinalysis. Culture examination is requisitioned if microscopy reveals significant number of pus cells (more than five) or history of urinary tract infection (UTI), especially in women with cystocele, urinary complaints and fistula.
Fasting and post-prandial blood sugar estimations.
Kidney function tests. Blood urea, serum creatinine and uric acid.
Liver function tests. Particularly in women giving a history of jaundice and in all women undergoing cancer surgery.
Blood tests for VDRL. Australia antigen and HIV-I and II.
Serum electrolytes. Na, K, Cl and HCO3.
Examination besides blood pressure. Pap smear is taken as required.
Postoperative Care: Postoperative care is important if surgical complications are to be avoided.
Immediate Care (24 H)
Vital signs such as
Pulse, temperature, BP and respiration chart to be maintained.
The patient needs intravenous fluid for 24 h. Following a minor surgery, oral fluids are allowed 4 h after the surgery, and soft diet is given on the day of surgery.
The average patient needs 2 L of fluid intravenously for 24 h. This comprises 1 L of 5% glucose, 1/2 L of glucose saline and 1/2 L of Ringer’s lactate to maintain electrolyte balance. If the woman vomits, extra fluid is required to make up for the loss.
Surgical Procedures: Dilatation of the Cervix and Endometrial Curettage (D&C)
D&C is a minor gynaecological procedure of dilatating the cervix and curetting (scraping) the endometrial tissue from the uterine cavity.
It is mainly a diagnostic procedure, rarely done for therapeutic purpose (mainly obstetric).
Dilatation of the cervix alone is required in the following conditions:
Ø Prior to curettage (commonest).
Ø For cervical stenosis.
Ø To prevent cervical stenosis following Manchester operation for prolapse of the uterus.
Ø To prevent postoperative cervical stenosis in cauterization of cervical erosion and conization.
Ø To drain haematometra.
Ø To drain pyometra.
Prior to insertion of radium into the uterine cavity in cancer of the cervix and endometrial cancer.
Prior to removal of embedded intrauterine contraceptive device (IUCD).
Prior to breaking uterine adhesions in Asherman syndrome.
Prior to endocervical curettage for endocervical cancer.
Prior to hysteroscopy.
Anesthetic Considerations for Complicated Pregnancies:
Substance abuse: has crossed social, economic, and geographic borders, and throughout the world, it remains one of the major problems facing society. The prevalence of substance abuse in young adults (including women) has increased markedly over the past 20 years. Almost 90% of drug-abusing women are of childbearing age.139-144 Substance abuse is “self-administration of various drugs that deviates from medically or socially accepted use, which if prolonged, can lead to the development of physical and psychological dependence.”
Related conferences:
Thyroid 2018, Conference on September 03-04, 2018 Auckland, New Zealand
Diabetes 2018, Conference on September 28-29, 2018 Montreal, Canada
Endocrinology Summit 2018, October 01-02, 2018 Osaka, Japan
Euro Endocrinology 2018, Meeting on November 26-27, 2018 Dublin, Ireland
Surgeons-2018, Symposium onNovember 22-24, 2018 Romania
Robotic Surgery 2018, Meeting on May 21-22, 2018 Tokyo, Japan
Anesthesiology-2018, Conference on November 15-16, 2018 Dubai, UAE
Surgery Asia Pacific 2018, Meeting on November 27-28, 2018 Singapore
Gynecology and Obstetrics Pathology 2018, Symposium on March 30-31, 2018 Orlando, USA
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Track 10: Menopause:
Menopause is also known as the climacteric, this is the time when menstrual cycles in women stop permanently, and they are no longer able to bear children. Typically menopause occurs between 49 to 52 years of age. Medical professionals often define menopause as having occurred when a women has not had any vaginal bleeding for over a year. The removal of the uterus, symptoms typically occur earlier, at an average age of 45 years. This may also be defined by a decrease in hormone production by the ovaries. For those who have had surgery to remove their uterus but still have ovaries, menopause may be viewed to have occurred at the time of the surgery or when their hormone levels fall.
Menopause is a natural change. This can occur earlier in those who smoke tobacco. Other causes include surgery that removes ovaries or chemotherapy. At the physiological level menopause happens due to production of the harmones estrogen and progesterone which results in the decrease of ovaries. Diagnosis of menopause is confirmed by measuring hormone levels in the blood or urine. Menarche is the opposite of menopause, the time when women’s periods start.
Specified treatment is not usually needed. Symptoms can be improved with treatment with respect to hot flashes, avoiding smoking, caffeine and alcohol is often recommended. Sleeping in a cool room with a fan may be suggested. There are some medications that may held such as menopausal hormone therapy (MHT), Clonidine, selective serotonin reuptake inhibitors or gabapentin. High-quality evidence for the effectiveness of alternative medicine has not been found. Exercise may help with sleeping problems. MHT was once routinely prescribed, it is now only recommended in those with significant symptoms.
Related conferences:
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan;
Gynecology 2018, Conference on July 23-24, 2018 Rome, Italy
Women’s Health 2018, Summit on July 18-19, 2018 Sydney, Australia
Health Care 2018, Conference on August 13-14, 2018 Bali, Indonesia
Thyroid 2018, Conference on September 03-04, 2018 Auckland, New Zealand
Diabetes 2018, Meeting on September 28-29, 2018 Montreal, Canada
Endocrinology Summit 2018, on October 01-02, 2018 Osaka, Japan
Euro Endocrinology 2018, Summit on November 26-27, 2018 Dublin, Ireland
Global Cancer 2018, Summit on March 12-14, 2018 Singapore
Epigenetics-2018, Conference on October 22-24, 2018 Turkey
Track 11: Maternal/Fetal medicine
This field of medicine is also known as perinatology and deals on managing the concerns of the mother and fetus during and shortly after pregnancy. The specialists who deal with Maternal-fetal medicine are generally with in the field of obstetrics. They act as consultants especially during high- risk and low-risk pregnancies. They work closely with paediatricians or neonatologists after birth. For the mother, they assist with pre-existing health concerns as well as complications caused by pregnancy.
These specialists attend to patients who fall within certain levels of maternal care where levels correspond to health risks for the baby, mother, or both during pregnancy. These specialists take care of women who are having hearth diseases, kidney diseases, hypertension, diabetes and thrombophilla. They also deal with mother’s pre-existing health conditions, such as blood pressure, dug use before and after pregnancy. In addition women facing difficulty with conceiving may be referred to a maternal-fetal specialist.
Amniotic Fluid Dynamics: Amniotic fluid (AF) is necessary for normal human fetal growth and development. It protects the fetus from mechanical trauma, and its bacteriostatic properties may help to maintain a sterile intrauterine environment. The space created by the AF allows fetal movement and aids in the normal development of both lungs and limbs. Finally, AF offers convenient access to fetal cells and metabolic by products and therefore has been used for fetal diagnoses more often than any other gestational tissue. The existence of AF has been appreciated since ancient times. Leonardo drew the fetus floating in the fluid, and William Harvey hypothesized that the fetus was nourished by it. Only in the late 19th century, however, did AF become available for study other than at delivery, and fl uid sampling by amniocentesis was rarely performed until the second half of the 20th century. Genetic amniocentesis for fetal sex determination was first performed in 1956.1 Research on the characteristics of AF is therefore a relatively recent development. This chapter reviews the current state of knowledge regarding the volume, composition, production, resorption, and volume regulation of AF.
Multiple Gestation:
Incidence of Twinning The incidence of twinning is increasing as our population ages and a new technology—assisted reproductive technology (ART)—is becoming widely used. Not only have artificial reproductive techniques led to a marked increase in higher-order multiple births (triplets, quadruplets) but also they are followed by an increase in prematurity rates and congenital anomalies.1-3 The statistics, which are usually derived from national or regional birth records and rely on reporting by physicians or other personnel attending births, do not accurately reflect the occurrence of twins at conception because the much higher prenatal mortality of twins (as abortion or fetus papyraceus) is not taken into account. Thoughtful reviews of the multiple gestation “epidemic” are available.4-6 Some countries have chosen to deny transfer of more than one blastocyst.7 An additional fi nding of interest is that there appears to be an increase in monozygotic twinning (identify-ed as being monochorionic) when various ART procedures are used; also, placental abnormalities are more frequent.8 Guttmacher9 suggested that 1.05% to 1.35% of pregnancies were twins, the reason for this wide variation being that the frequency of the twinning process varies widely among different populations. Data collated from various countries reveal that the variability relates largely to the ethnic stock of the population under consideration. Moreover, although the dizygotic (DZ) twinning rate varies widely under different circumstances, the monozygotic (MZ) twinning rate is considered to be “remarkably constant,” usually between 3.5 and 4 per 1000,10 although Murphy and Hey11 found the rate to have slightly increased in recent years. In recent national statistics, of 4 million births in the United States, 3.3% were multiple or 1 in 30 gestations. When the twinning rate of a population is known, the frequencies of triplets, quadruplets, and so on can be roughly calculated by Hellin’s hypothesis, which states that when the frequency of twinning is n, that of triplets is n2 , of quadruplets n3 , and so on. The highest number recorded so far is nine offspring.12 Since 1973, there has been a steady rise in the incidence of twins and triplets, so that currently at least 1 in 43 births is a twin and 1 in 1341 pregnancies results in triplets.2,13 In part, this increase was attributed to delayed childbearing, but the use of ovulation-enhancing drugs has also been implicated. Although acknowledging the increased DZ twinning frequency attributed to clomiphene, Tong and coworkers14 found that the DZ-to-MZ ratio has significantly declined from 1.12 (1960) to 0.05 (1978) and suggested adverse environmental factors as a possible cause.
Abnormalities of Twin Gestation
Fetus Papyraceus: When one or more of the fetuses in a multiple gestation dies before birth and the pregnancy continues, the fluid of the dead twin’s tissues is gradually absorbed, the amniotic fluid disappears, and the fetus is compressed and becomes incorporated into the membranes. Hence, it is called a fetus compressus, fetus papyraceus, or membranous twin. The condition occurs in both DZ and MZ twins and is a regular fi nding when multiple gestations are surgically reduced. This has become much more common in recent years as many fetuses are conceived with ART. Acardiac Twin: The most bizarre malformation recorded, acardiac twin, occurs only in one twin of a pair of MZ twins.
Related conferences:
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Advanced Nursing Science 2018, Conference on April 20-21, 2018 Las Vegas, USA
Nursing & Healthcare Congress 2018, on April 23-25, 2018 Dubai, UAE
Neonatal Nursing Congress 2018, on May 14-15, 2018 Singapore
Midwifery Congress 2018, on May 11-12, 2018 Osaka, Japan
Gynecology and Obstetrics Pathology 2018, Conference on March 30-31, 2018 Orlando, USA
Midwifery 2018, Summit on September 26-27, 2018 Chicago, USA
Breast Pathology 2018, Conference on June 25-26,2018 Vancouver, Canada
Nursing Global 2018, Summit on March 01-03, 2018 London, UK
Track 12: Reproductive endocrinology and infertility
Reproductive Medicine: this is a branch of medicine which deals with inhibition and identification of reproductive problems. This is found on awareness of reproductive anatomy, endocrinology and physiology, which incorporates relevant aspects of molecular affinity, pathology and biochemistry. In women menstruation is also covered in reproductive medicine.
Reproductive medicine addresses the issues of puberty, sexual education, family planning, reproductive system disease, infertility etc. Including sexual dysfunction in women.
This surgical subspecialty in obstetrics and gynecology trains physicians in reproductive medicine addressing hormonal functioning as it pertains to reproduction as well as the infertility. Most of the specialists focus on the treatment of infertility. RE (Reproductive Endocrinologists) are trained to treat males and females outside infertility. RE’s have specialty training in obstetrics and gynecology before they undergo sup-specialty training in REI.
Related conferences:
Herbal Diabetes 2018, Conference on August 20-21, 2018 Singapore
Diabetes Asia Pacific 2018, Meeting on July 16-17, 2018 Sydney, Australia
Diabetes Global 2018, Summit on March 8-9, 2018 | Paris, France
Diabetes Europe 2018, Symposium on June 20-21, 2018 | Rome, Italy
Diabetologists 2018, Conference on May 23-24, 2018 New York, USA
Metabolic Syndrome 2018, Conference on June 28-29, 2018 Amsterdam, Netherlands
Thyroid 2018, Summit on September 03-04, 2018 Auckland, New Zealand
Diabetes 2018, Conference on September 28-29, 2018 Montreal, Canada
Endocrinology Summit 2018, on October 01-02, 2018 Osaka, Japan
Euro Endocrinology 2018, Summit on November 26-27, 2018 Dublin, Ireland
Track 13: Urogynecology/reconstructive pelvic surgery
This is a sub-specialty of urology and gynecology. The international Urogynecological Association (IUGA) is a global body for professionals those who are practicing in the field of urogynecology, female pelvic medicine, and reconstructive surgery. IUGA also provides educational opportunities for urogynecologists both online and in-person, develops terminology and standardization for the field. The other international organization is ICS (International Continence Society) which strives to improve the quality of life for people affected by urinary, bowel and pelvic floor disorders through education, and research.
In some countries this sub-speciality is also known as the Pelvic Medicine and Reconstructive surgery. The urogynecologist manages clinical problems associated with dysfunction of the pelvic floor and bladder. The pelvic floor disorders affect the reproductive organs, bladder and bowels. Some common disorders include. Urinary incontinence, pelvic organs prolapse and faecal incontinence. Some conditions treated in urogynecology practice include:
|
Female genital prolaspse Enterocele Cystocele Fecal incontinence Lichen planus Lichen sclerosus Overactive bladder Pelvic organ prolapse Rectocele Urinary incontinence Urinary retention Vaginal agenesis Vaginal septum Vesicocutaneous fistula Vesicouterine fistula Voiding difficulties Viscovaginal fistula etc…. Speciality treatments available include: Abdominal reconstruction |
Behavioural modification Biofeedback Dietary modification Fascial grafts Laparoscopic reconstruction Pessary Pelvic floor re-education Relaxation techniques Robotic reconstruction Urethreal injections Vaginal reconstruction etc…
|
Related conferences:
Robotic Surgery 2018, Summit on May 21-22, 2018 Tokyo, Japan
Anesthesiology-2018, Conference on November 15-16, 2018 Dubai, UAE
Surgery Asia Pacific 2018, Meeting on November 27-28, 2018 Singapore
Bariatric Surgery 2018, Conference on March 15-16, 2018 Barcelona, Spain
Anesthesiology 2018, Conference on September 17-18. 2018 Dubai, UAE
Surgery Congress-2018, on August 27-28, 2018 Tokyo, Japan
Surgeons-2018, Meeting on November 22-24, 2018 Romania
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Breast Pathology 2018, Conference on June 25-26, 2018 Vancouver, Canada
Track 14: Menstruation
This is also known as period or monthly. This is the monthly discharge of blood and mucosal tissue form inner lining of the uterus through vagina. Usually at the age of twelve and fifteen the first period occurs which is known as menarche. Sometimes period may occur occasionally at the age of eight years and considered normal. Menstruation stops occurring after menopause, which is usually occurs between 45 and 55 years of age. Periods also stop during pregnancy. The lack of periods, known as amenorrhea, when periods do not occur by age 15 or have not occurred in 90 days. Other problem in menstrual cycle includes painful periods and abnormal bleeding such as bleeding between periods or heavy bleeding. Health effects in menstruation such as cramps, mood and behaviour, bleeding, in some cases stronger physical and emotional sensations may interfere with normal activities and include menstrual pain, migraine headaches and depression. Severe uterine pain or Dysmenorrhea is common in young females.
|
Symptom |
|
|
Infrequent periods |
Oligomenorrhea |
|
Short or extremely light periods |
Hypomenorrhea |
|
Too-frequent periods (defined as more frequently than every 21 days) |
Polymenorrhea |
|
Extremely heavy or long periods (one guideline is soaking a sanitary napkin or tampon every hour or so, or menstruating for longer than 7 days) |
Hypermenorrhea |
|
Extremely painful periods |
Dysmenorrhea |
|
Breakthrough bleeding (also called spotting) between periods; normal in many females |
Metrorrhagia |
|
Absent periods |
Amenorrhea |
Related conferences:
Gynecology and Obstetrics Pathology 2018, Conference on March 30-31, 2018 Orlando, USA
Midwifery 2018, Summit on September 26-27, 2018 Chicago, USA
Midwifery Congress 2018, on May 11-12, 2018 Osaka, Japan
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Health Care 2018, Congress on August 13-14, 2018 Bali, Indonesia
Health Economics Congress 2018, on September 13-14, 2018 Zurich, Switzerland
Health Economics 2018, Conference on April 12-13, 2018 Amsterdam, Netherlands
Public Health 2018, Summit on February 26-28, 2018 London, UK
Neonatal 2018, Symposium on June 27-28, 2018, Vancouver, Canada
Track 15: Sexual Medicine and Infectious Diseases in Gynecology (Acute and chronic)
Sexual development: the development of normal male and female genital organs and tracts is determined by several factors, all of which are time specific during embryogenesis. The critical period for gonadal development is at 6-7 weeks of embryogenesis when Y chromosome promotes male gonadal development. The external genital organs start developing at 10th week and reach completion by 16th week. The genetic sex is determined at fertilization, but the gonads remain undifferentiated until 6 weeks of intrauterine life. Fist the sex chromosomes determine into a testis or ovary. Y chromosome develops a male gonad and absence of Y and presence of XX chromosome ovaries. If the gonad is male, genes associated of the somatic cells in the primitive gonad and initiate development along the male lines. The elaboration of the H–Y antigen complex in the short arm of Y chromosome known as sex-determining region Y (SRY) induces testicular development. The Sertoli cells in the developing testis produce Müllerian-inhibiting substance (MIS) that causes regression of the Müllerian (paramesonephric) ducts. In the absence of MIS, Müllerian ducts develop passively to form the fallopian tubes, uterus and upper vagina. Female internal organs and external genitalia develop partially without the need for ovarian hormones and differentiate even in the absence of the gonads, unless interrupted by the regressive influence of MIS. Differentiation of the Müllerian ducts proceeds cephalocaudally to form the female internal genital organs. In the absence of the masculinizing
Components Contributing to Determination of Sex:
Genetic Sex: In each individual, the nuclei of humans contain a diploid number of chromosomes, 22 pairs of autosomes and 1 pair of sex chromosomes, making a total of 46. During maturation, a reduction division results in each ovum or spermatozoon containing only the haploid number of 22 unpaired autosomes and 1 sex chromosome. In the ovum, the sex chromosome is always X, but in the sperm, it is either X or Y. The relative number of X- and Y-carrying spermatozoa is equal. As the spermatozoon carries either an X or a Y chromosome, fertilization results in a 46-chromosome pattern carrying either an XX or XY – a genetic female or a genetic male, respectively. Thus, the original diploid number of chromosomes is restored (22 pairs of autosomes plus the paired sex chromosomes – 46 in all). The genetic sex of an individual is determined at fertilization. In the fertilized egg, the Y chromosome directs the development of the undifferentiated gonads into testes and absence of Y into ovaries 2 weeks later. The ovaries do not participate in sexual development. Y chromosome contains on its short arm H–Y antigen (surface SRY cell antigen), which is responsible for the development of testes. The autosomes also take part. This Y chromosome has no further influence beyond the development of the gonads. The germ cells arise in the endodermal wall of the primitive gut near the yolk sac from where they migrate along the dorsal mesentery into the gonadal site. The Leydig cells (interstitial cells) produce testosterone that develops the Wolffian duct and urogenital sinus into male genital organs and external genitalia. External Anatomical Sex The shape of the body contours, the development of the musculature, the characteristics of the bones (notably the pelvis), the distribution of hair on the face and body, breast development and the external genitalia are strong presumptive evidence of either sex. Internal Anatomical Sex The presence of a recognizable uterus, fallopian tubes and ovaries is the evidence that the individual is a female. The rare exception is the true hermaphrodite. Gonadal Sex Gonadal sex depends on the histological appearance of the gonad from the study of a biopsy or the removal of the organs. It is not entirely diagnostic such as in the case of an ovotestis in which both female and male elements are histologically demonstrated. Also, it is possible to have a rudimentary testis on one side and a rudimentary ovary on the other. Such findings are, however, so rare that the sex of the gonad is a reasonably reliable guide to the true sex of an individual. Hormonal Influences In the female pseudohermaphrodite, an excess production of androgenic hormone by adrenal cortical hyperplasia can modify the external genitalia of a genetic female. Hypertrophy of the phallus and fusion of the labia majora may cause the parents to consider their child to be a male. The virilizing tumours of the ovary, such as arrhenoblastoma, can cause hirsutism, hypertrophy of the clitoris, deepening of the voice, masculine body contours and amenorrhoea. The presence of oestrogen in the male can cause gynaecomastia. These are all examples of how hormones, natural or exogenous, can modify the sexual organs and secondary sexual characteristics.
Feminism
Swyer’s Syndrome
Turner’s Syndrome
Masculinism
Klinefelter Syndrome
Virilism
Hirsutism
Hirsutism is defined as distribution of coarse hair in a female normally present in a male, i.e. upper lip, chin, chest, lower abdomen and thighs. Hirsutism may or may not be associated with menstrual disturbances such as oligomenorrhoea and amenorrhoea. Virilization refers to a condition of hirsutism associated with other male characteristics such as temporal baldness, hoarse voice, clitoromegaly and muscle enlargement as well as defeminization such as amenorrhoea and breast atrophy
Causes of Hirsutism
Ø Genetic and ethnic.
Ø Excess androgen or increased sensitivity of the pilosebaceous unit to T.
Ø Liver disease when the level of SHBG level drops.
Ø Ovarian. Polycystic ovarian disease (PCOD), hyperthecosis, masculinizing ovarian tumours, e.g. arrhenoblastoma, hilus cell tumour.
Ø Adrenal. Congenital adrenal hyperplasia, Cushing’s syndrome, adrenal tumour (1%–2% cases).
Ø Drugs. Androgens; progestogens with androgenic effect, viz. 19-norsteroids, and levonorgestrel nabolic steroids, phenytoin, danazol, minoxidil.
Ø Others. Obesity, hypothyroidism, anovulatory hypooestrogenism, idiopathic – 15%, hyperprolactinaemia.
Ø Hirsutism occurs early in congenital adrenal hyperplasia, around puberty in PCOD and in elderly women at menopause.
Vulvar Infections: The normal vulva is composed of the skin consisting of stratified squamous epithelium. It contains sebaceous, sweat and apocrine glands, underlying subcutaneous tissue and the specialized Bartholin’s glands. Vulvar pruritus and burning account for approximately 10–15% of presenting complaints
Molluscum Contagiosum It is a benign viral infection caused by the poxvirus. It is spread by close sexual or nonsexual contact and by autoinoculation. The incubation period ranges from several weeks to months
Scabies Itch mite: It is transmitted through close contact/fomites.
Condylomata Acuminata Also called venereal warts, these are caused by the HPV, which is a small DNA double-ended virus. These warts spread diffusely over the whole of the vulval area. The verrucous growths may appear discrete or coalesce to form large cauliflower-like growths. They affect the skin of the smeared with water-soluble K-Y jelly and treated with dilute acetic acid. The vascular pattern is studied. The abnormal areas stained with toluidine blue are biopsied.
Related conferences:
Std Asia Pacific 2018, Summit on August 22-23, 2018 Tokyo, Japan
STD-AIDS-2018, Congress on May 30-31, 2018 Auckland, New Zealand
Bacteriology 2018, Conference on May 21-22, 2018 New York, USA
Infection Congress 2018, on March 1-2, 2018 Berlin, Germany
Bacteriology Congress 2018, on June 04-05, 2018 Osaka, Japan
HIV/AIDS MEET 2018, on August 20-21, 2018 Prague, Czech Republic
Infectious Diseases Congress 2018, on July 26-27, 2018 Melbourne, Australia
Infectious Diseases 2018, Congress on September 17-18, 2018 San Diego, USA
Infectious Diseases 2018, Conference on October 15-16, 2018, Abu Dhabi, UAE
Neglected Tropical Diseases 2018, Summit on August 29-30, 2018 | Boston, USA
Track 16: Therapies in Gynecology
Therapies in gynecology are Radiotherapy, Chemotherapy, Immunotherapy and Genetherapy. Pre-treatment evaluation and proper monitoring during therapy are mandatory to prevent or minimize the toxicity. Growth factors or granulocyte colony-stimulating factor are used to prevent hemorrhagic toxicity of chemotherapy. Multiple chemotherapeutic agents have been used to kill cancer cells, they have also been used to sensitize cells to radiation. Chemoradiation improves outcome especially with squamous cell cancers.
Radiotherapy and chemotherapy are the important modalities of therapy for human cancers apart from sugery. Bias towards any particular one is unscientific. They may have a curative role when used as a primary therapy. Multidisciplinary approach is needed for the treatment of some malignancies to improve the outcome. Radiotherapy and chemotherapy should be considered even for palliation of incapacitating symptoms when cure may not be achieved.
Ionizing radiation used for therapy may be 1. Electromagnetic radiation 2. Particulate radiation.
Techniques of Radiation Therapy
Ø Brachy Therapy
Ø Particulate Radiation
Ø After Loading Technique
Ø External Beam Radiotherapy
Ø Intensity Modulated Radiation Therapy
Ø Three-dimensional Conformal Radiation Therapy (3D CRT)
Immunotherapy in Gynecology:
Approaches to augment the immune response to human tumour include: Active immunotherapy and Passive Immunotherapy. Immunotherapy in malignancy-is being explored recently. Cytokines (Polypeptides) have antitumor and immune stimulating effects. Augmentation of immune system is achieved by active (interferon, IL-2) and passive immunotherapy
Active Immunotherapy (to induce host immune response).
Biological immunostimulants—administration of BCG (Bacille Calmette-Guerin), C parvum (Corynebacterium parvum).
Chemical immunostimulants—Levamisole, cimetidine.
Cytokines, interferons (IFN), interleukine (IL-2), and tumor necrosis factor (TNF)
Chemotherapeutic drugs—cisplantin, doxorubicin
Passive immunotherapy (Immunologically active substances are directly transferred to the host)
Ø Cytokines: Interferon, TNF.
Ø LAK cells: Together with IL-2
Ø Monoclonal antibodies
Ø Activated macrophages: Interferon
Ø Immunotherapy has its limitations. Immune response enhancement leading to rejection of tumor can occur when the following conditions are fulfilled:
Ø Biological response modifiers are indirect contact with tumor’s
Ø Tumor bulk is minimal
Ø Blood supply is good
Ø Monoclonal antibodies to be conjugated with agents (Chemotherapy drugs, toxins, interferon) for precise delivery to tumor cells
Genetherapy: the effect of oncogene function can be transformed by two approaches. One attempt is to remove the oncogene product or to block its function. Alternatively, one can use antisense oligonucleotides in an attempt to block the production of oncogene by preventing the transcription of chromosomal DNA to RNA. Antisense oligonucleotide can be administered systematically. Cytokine gene transfer to tumour cells. Cells are engineered to produce cytokines including interleukines 2, 4, 5 and 6 TNF and others. Clinical trials are in progress in patients with squamous cell carcinoma,
Familial cancer (breast, ovary, and colon) is explained on the basis of genes (oncogene, tumor suppressor gene and mutator gene). Point mutation, deletion and insertion are the important changes. Gene therapy to the tissues at risk by insertion of normal copies of genes is a way forward.
Tumor Markers: indicate the presence and also the site of tumor. It is useful in screening, diagnosis and management of cases and also for follow up. Gynecological tumor markers in common use are—hCG in trophoblastic tumor, AFP in germ cell tumor, CA-125 in ovarian epithelial tumor and SCC in carcinoma cervix HER-2/ner, an oncogene product is used for epithelial ovarian cancer.
Related conferences:
Cancer Science 2018, Summit on August 09-10, 2018 Madrid, Spain
Cancer Congress 2018, on September 17-18, 2018 San Diego, USA
Cancer 2018, Congress on October 03-04, 2018 Los Angeles, California, USA
World Cancer 2018, Summit on October 11-13, 2018 Zurich, Switzerland
Cancer Therapy-2018, Conference on October 29-30, 2018 San Francisco, California, USA
World Cancer 2018, Summit on July 02-03, 2018 Thailand, Bangkok
Medical Oncology-2018, Conference on May 28-30, 2018 Osaka, Japan
Clinical Oncology-2018, Congress on June 1-2, 2018 Osaka, Japan
Global Cancer 2018, Summit on March 12-14, 2018 Singapore
Epigenetics-2018, Conference on October 22-24, 2018 Turkey
Track 17: Contraception and Family Planning
Rapid population growth is a critical issue worldwide. Family planning matters save women’s lives preventing unintended pregnancies. Slower population growth conserves resources, improves health and living standards. Benefits of fertility control are interrelated. Benefits are: improved quality of life, better health, less physical and emotional stress of life, better education, job and economic opportunities. Benefits are enjoyed by the couple, the children, other family members, the community and the country. Contraception and fertility control are not synonymous. Fertility control includes both fertility inhibition and fertility stimulation. While the fertility stimulation is related to the problem of the infertile couples, the term contraception includes all measures, temporary or permanent, designed to prevent pregnancy due to the coital act. Methods of contraception are two types Temporary and Permanent. Temporary includes Barrier methods, Natural Contraception, Intrauterine contraceptive devices (IUCD’s). Permanent methods include Tubal occlusion for female and Vasectomy for males.
Intrauterine Contraceptive devices: is a widely acceptable reversible method of contraception for spacing of births, amongst many, either a copper impregnated device like Cu T, multi load or a hormone releasing device like LNG-IUS induces uniform suppression of endometrium and produces very scanty cervical mucus. It should not be used in newly married women or when any pelvic pathology is present. The device can be introduced in the interval period of following abortion or following childbirth. The introduction is an outdoor procedure and can be done even by trained paramedical personnel without anesthesia. The technique employed is either push-out in Lippes loop or “withdrawl” in Cu T. The immediate complications include cramp-like pains or even syncopal attacks. The delayed complications include pelvic pain, menstrual irregularities, and expulsion of the IUD or even Perforation of the uterus. Complications are much less with third generation of IUD’s.
Steroidal Contraception’s
Enovid was used in the first contraceptive field trial in Puerto Rico in 1956 by Pincus and his colleagues. Intensive pharmacological research and clinical trials were conducted during the following years to minimize the adverse effects of estrogen without reducing the contraceptive efficacy, resulted in lowering the dose of estrogen to minimum of 20ug or even 15 ug in the tablet
Progestin only contraception (POP/MINI PILL)
POP is devoid of any estrogen compound, it contains very low dose of a progestin in any one of the following form –Levonorgestrel 75ug, norethisterone 350ug. Desogestrel 75ug, lynestrenol 500ug, or norgestrel 30ug. It has to be taken daily form the first day of the cycle.
Injectable Progestin’s
The preparations commony used are depomedroxy progesterone acetate (DMPA) and norethisterone enanthate (NET-EN). Both are administered intramuscularly within five days of the cycle. The injection should be deep. Z-tract technique and the site not to be messaged. DMPA in a dose of 150mg every months or 300mg every six months; NET-EN in a dose of 200mg given at two-monthly intervals.
Emergency Contraception’s (EC): emergency contraception include the following
Harmones
IUD
Anti-Progesterone
Others
Sterilization: permanent surgical contraception, also called voluntary sterilization, is a surgical method whereby the reproductive function of an individual male or female is purposefully and permanently destroyed. The operation done on male is vasectomy and that on the female is tubal occlusion, or tubectomy.
Couple must be counselled adequately before any permanent procedure is undertaken. Individual procedure must be discussed in terms of benefits, risks, side effects, failure rate and reversibility. Vasectomy is a permanent sterilization operation done in male where segments of vas deferens of both the sides are resected and the cut ends are ligated. Other methods to block the Vas are Electrocoagulation: May be used to encourage scar tissue formation and Fascial interposition: following ligation, excision and cautery. This is done to prevent recanalization
Tubectomy: in this operation where resection of a segment of both the fallopian tubes is done to achieve permanent sterilization. The approach may be Abdominal or Vaginal
Laparoscopic Sterilization is the commonly employed method of endoscopic sterilization. It is gradually becoming more popular—especially, in the camps. The procedure is mostly done under local anesthesia. The operation is done in the interval period, concurrent with vaginal termination of pregnancy or six weeks following delivery. It should not be within following delivery.
Related conferences:
Advanced Nursing Science 2018, April 20-21, 2018 Las Vegas, USA
Nursing & Healthcare Congress 2018, on April 23-25, 2018 Dubai, UAE
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Women’s Health 2018, Congress on July 18-19, 2018 Sydney, Australia
Health Care 2018, Summit on August 13-14, 2018 Bali, Indonesia
Health Economics Congress 2018, on September 13-14, 2018 Zurich, Switzerland
Health Economics 2018, Conference on April 12-13, 2018 Amsterdam, Netherlands
Public Health 2018, Summit on February 26-28, 2018 London, UK
Neonatal 2018, Conference on June 27-28, 2018, Vancouver, Canada
Track 18: Midwifery
This is the health science and profession which focuses on pregnancy, childbirth and postpartum period besides reproductive and sexual health. This is independent and direct specialization in education in many countries and it is not a medical speciality. Midwives are recognized as highly trained and specialized professionals in obstetrics. This track focuses on the challenges of the midwifes in the field of Gynecology and women healthcare management
Related conferences:
Midwifery 2018, Summit on September 26-27, 2018 Chicago, USA
Neonatal Nursing Congress 2018, on May 14-15, 2018 Singapore
Nursing Global 2018, Summit on March 01-03, 2018 London, UK
Nursing & Healthcare Congress 2018, on April 23-25, 2018 Dubai, UAE
Women’s Health 2018, Summit on July 18-19, 2018 Sydney, Australia
Advanced Nursing Science 2018, Conference on April 20-21, 2018 Las Vegas, USA
Breast Cancer 2018, Summit on May 10-11, 2018 Frankfurt, Germany
Gynecology and Obstetrics Pathology 2018, Conference on March 30-31, 2018 Orlando, USA
Gynecology Congress 2018, on August 22-23, 2018 Tokyo, Japan
Gynecologic Congress 2018, on July 23-24, 2018 Rome, Italy
Market Analysis
Market Analysis
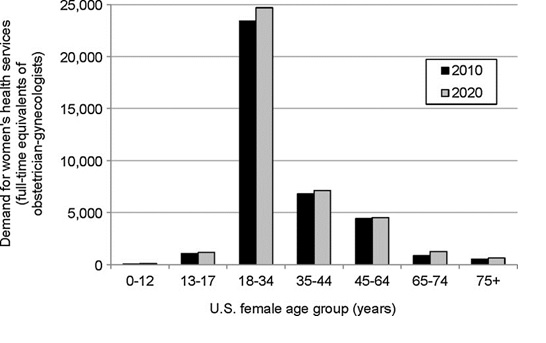
The demand for women’s healthcare is estimated to only increase by 2020. Based on the length and expense required to train new physicians, it is anticipated in advance for any imbalances between the supply and demand for women’s healthcare providers. To estimate the requirement of physicians, sometimes physician to population rations are used to determine the requirement of physicians in regions, along with many factors affecting current and future demands of women’s healthcare. Adequate supply and demand of providers are also essential to maintain optimal healthcare for women.
Many factors that are considered to determine the demand for women healthcare are female population, cultural, economic and health risk factors. These factors are considered as the endpoints to measure the use and to deliver the healthcare services. The unique way to quantify the healthcare demands to women is only by examining the use of obstetrics and gynecology services. Based on which we can estimate the demand for obstetrics and gynecological services between 2010-2020. 37,370 physicians were engaged in women’s health care activities in 2010. The total patients calculated were 59% at physician’s offices. 29%patients were estimated in the operating room or labour and delivery unit,
During 2015, the postmenopausal osteoporosis segment dominated the market and accounted for more than 37% of the market share. Factors such as the rising number of older people worldwide. Women above 50 are likely to be affected with postmenopausal symptoms due to various hormonal changes. According to the International Osteoporosis Foundation, it is expected that close to 200 million women will be affected by postmenopausal osteoporosis globally, thereby spurring the growth of this market segment over the forecast period.
Market research analysts have predicted the global women’s health market to grow at a CAGR of more than 3% over the forecast period. With many countries improving the healthcare facilities, the market for women’s health will have a positive outlook in the coming years. Many countries have substantially increased their healthcare budgets as a part of their social security measure. For instance, the US government spend 17% of their GDP on the healthcare sector in 2014. With increases in the budgets by many countries, the women’s health market is expected to show positive rise until the end of 2020.

In this industry research report, the analysts have estimated factors such as the growing awareness of birth control methods will spur the growth of this market in the forecast period. Contraception and fertility control are supported by the governments of developing nations such as India and China to curb the growing population. However, in western countries women have stopped using contraceptive pill due to their side effects and are increasingly using IUDs and implants. Therefore, the increasing awareness about alternative growth methods will aid in the growth of this market until the end of 2020.
In 2015, the global women’s heath market was led by the Americas accounting for close to 40% of the market share. The region is exhibiting consistent growth because of the increasing population of older women affected by diseases such as breast cancer, endometriosis, and postmenopausal osteoporosis. Moreover, the presence of several labs and research facilities in the region will also drive this market’s growth in the Americas.
Past Conference Report
Gynecology 2017
Past Reports Gallery
To Collaborate Scientific Professionals around the World
Conference Date September 28-29, 2018
For Sponsors & Exhibitors
Speaker Opportunity
Useful Links
Past Conference Report
Supported By
All accepted abstracts will be published in respective Conference Series International Journals.
Abstracts will be provided with Digital Object Identifier by




